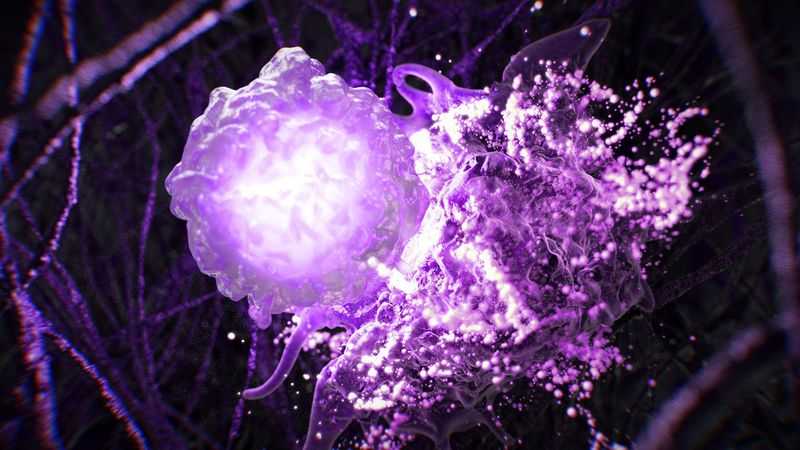
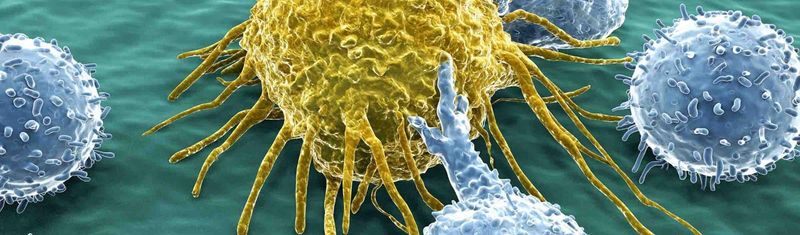
Immunotherapies have been successful in the targeted treatment of cancer, but we have still only scratched the surface. Our immuno-oncology teams are leveraging immunoscience to better detect and attack tumors, including harnessing more targeted approaches that weaponize the immune system against cancer without triggering an unwanted immune response.

Our Oncology Pipeline
We have more than a dozen next-generation molecules in the clinic, each with a distinctive mechanism of action against either hematologic malignancies or solid tumors.
Follow the Science
Our R&D teams follow the science to find treatments for people living with cancer.

Voices from the Lab: Nizar El Murr on Immuno-oncology
Our Multi-Front Attack on Cancer
John Reed and Frank Nestle discuss how we’re building an R&D pipeline to address critical gaps in cancer care
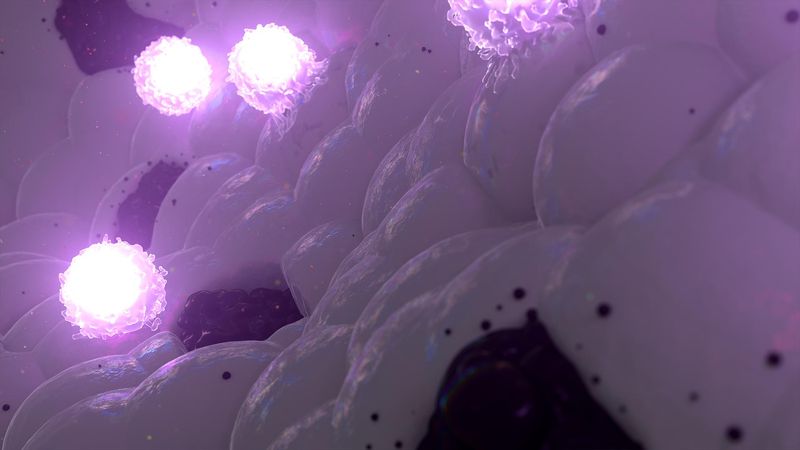
Bolstering the Immune System
Our immuno-oncology teams are working on ways to boost the immune system to better detect and attack tumors. And our molecular oncology teams are designing powerful precision drugs to either destroy cancer cells or activate immune cells locally.
Rethinking Oncology Drug Development
Our culture of collaboration empowers our teams to achieve real change for people battling cancer.
Technology Toolbox
We’ve reshaped our footprint in oncology, expanding our capabilities with state-of-the-art technologies in immuno-oncology, molecular oncology, and genomic medicine.

Collaboration
To further our bold vision of generating multiple candidates every year, we collaborate with innovative partners to break new ground in oncology.

Patient Centricity
By listening, learning, and keeping patients at the center of everything we do, we can advance the science and make a lasting difference in people’s lives.
More About Oncology
Cancer Under Siege
Our Commitment to Oncology

Your Health: Oncology
Our Latest Science Stories

February 24, 2026
AI Across the R&D Value Chain: Portfolio Decision-Making
More for Healthcare Professionals
Our Data-sharing Commitments
Our Disclosure Commitments
Find a Clinical Trial
Campus Sanofi
Selected publications
- LaMarche MJ (2022) Think Biologically, Act Chemically. J Medicinal Chem; DOI: 10.1021/acs.jmedchem.2c01121
- Manandhar M, Chun E, Romesberg FE (2021) Genetic Code Expansion: Inception, Development, Commercialization. J Am Chem Soc 143:4859-4878; DOI: 10.1021/jacs.0c11938
- Mitra-Kaushik S, Mehta-Damani A, Stewart JJ, et al. (2021) The Evolution of Single-Cell Analysis and Utility in Drug Development. AAPS J 23:98; DOI: 10.1208/s12248-021-00633-6