In the Spotlight

Our Science
October 8, 2025
Modulus: Redefining the Future of Biopharma Manufacturing

Our Science
July 9, 2025
AI Across the R&D Value Chain: Drug Discovery
Your Health
November 12, 2025
COPD Around the World: The Impact on Patients and Caregivers
Watch Our Latest Videos

How is AI Speeding up Drug Discovery?

Is AI a Superpower?

Caring with Courage

The Sanofi Connection
All Stories
Year
Topic
Our Science
January 6, 2026
Our Human-Centric Approach to Partnership Amidst an Evolving Biotech Landscape
Your Health
January 6, 2026
Defining a Clearer Path Forward in CIDP: Why Language Matters
Your Health
December 17, 2025
The Cause of COPD You Don't Know: Alpha-1 Antitrypsin Deficiency
Sustainability
November 24, 2025
Greener Science for a Healthier Planet: Sanofi & My Green Lab
Your Health
November 20, 2025
Breaking Barriers in Diabetes, Transforming Care Together
Your Health
November 13, 2025
How ITP Taught Me That My Voice Matters: My Journey from Silence to Advocacy
Your Health
November 12, 2025
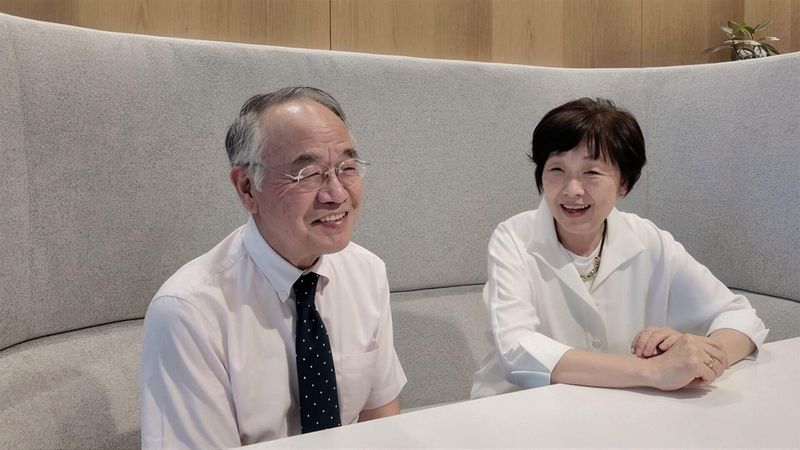
COPD Around the World: The Impact on Patients and Caregivers
Our Science
November 7, 2025
Helping Patients Breathe Better: Addressing Unmet Needs in Respiratory Care
Your Health
November 3, 2025
