Helping Patients Breathe Better: Addressing Unmet Needs in Respiratory Care
The treatment of respiratory diseases has improved over the last 50 years, but despite progress made, including the development of biologic treatments, there continue to be considerable unmet needs and massive challenges that have not been addressed.1 With our deep legacy in immunology and unrivaled expertise in immunoscience, we’re embarking on our next ambition: advancing a robust pipeline of potentially paradigm-shifting treatments that aim to revolutionize respiratory care across the spectrum of disease.
Our immune system is incredibly complex: it protects, modulates and arms us. We believe that deepening the understanding of how our immune system works for us – and sometimes against us – can help us combat many diseases.
At Sanofi, we have longstanding expertise in vaccines that involve the immune system response, and we have developed treatment options that sparked a paradigm shift in how we address specific chronic inflammatory diseases, such as asthma, atopic dermatitis (AD), eosinophilic esophagitis (EoE) and chronic rhinosinusitis with nasal polyposis (CRSwNP). We are studying the pathways, cell types and interactions that make up the immune system to identify the broader mechanisms that could help us combat disease. These pathways have led us to explore new investigational treatments across a number of chronic inflammatory diseases, including chronic obstructive respiratory disease (COPD), asthma and other respiratory diseases, which could one day potentially revolutionize care for patients.
The Substantial Burden of Chronic Respiratory Conditions
Chronic respiratory conditions, including asthma, COPD and CRSwNP, can manifest through severe, chronic and progressive symptoms, taking a significant toll on a person’s ability to breathe comfortably and live life free from the burden of their disease. Until a few years ago, there were limited advanced therapies available to treat patients suffering from severe respiratory diseases.
“I once had a patient in her forties with severe asthma. Not many treatment options were available back then – she was taking steroids and had to come back and forth to the hospital. The medication had side effects and her symptoms would recur, so she waited longer and longer until her attacks would return. One time, she waited too long and sadly passed away,” shared a Sanofi researcher and former physician. “It is stories like hers that made me realize how critical scientific research in immunology is to help to advance diverse treatment options.”
When it comes to sheer physical ability, nothing hinders the body quite like the inability to breathe properly. Chronic respiratory diseases have a significant physical, psychological and economic impact on patients and caregivers, as well as an economic burden on the healthcare system.

Shifting the Treatment Paradigm in Respiratory Diseases
At Sanofi, we have longstanding expertise in immunology research that has helped spark a paradigm shift in how we address specific chronic inflammatory diseases, including respiratory conditions. Through innovation, we, alongside our partner Regeneron, have significantly advanced care across chronic respiratory diseases with Type 2 inflammation, providing new solutions for the treatment of some of these diseases, including the emergence of biologic treatments.
But chronic respiratory conditions are complex and heterogenous. With the evolution of research in the field, it has become clear that there is a broad spectrum of inflammation underlying these conditions, and they are often driven by multiple pathways that can differ from person to person. Because of this, not all patients have the same response to treatment and may have different clinical presentations. This means the next frontier in immunology requires us to look beyond Type 2 inflammation.
Through our research and robust pipeline, we are pursuing diverse solutions, exploring novel pathways and modalities and seeking to help broader patient populations, including those with less severe disease, hard-to-treat conditions or those who do not respond to current treatments. By advancing innovative science, we aim to raise efficacy ceilings, intervene earlier in the disease, modify disease progression, and tailor treatment to patient needs.
Ultimately, our goal is to redefine the treatment paradigm in chronic respiratory disease and move toward a future where we treat these conditions with a personalized approach, addressing the specific underlying disease mechanisms driving each patient's condition.
We need more options for people who do not respond to current treatments. It is not enough to say ‘most’ people respond. It will only be good enough when everyone has a functional treatment that works for them.

Houman Ashrafian
Executive Vice President, Head of Research and Development
Driving Scientific Research to Address Unmet Needs in Respiratory Diseases
Across chronic respiratory conditions, we are exploring – and combining – a multitude of different pathways that could one day fill longstanding gaps in care.
For instance, in asthma, some patients exhibit potential evidence of mixed-type inflammation defined by both elevated neutrophils and eosinophils, which may add an additional layer of complexity to their care. Sanofi is exploring the potential of OX40-Ligand (OX40L), a key immune regulator12, as a target to stop inflammation at its root.13 The OX40L pathway may potentially impact patients with mixed inflammation, and that which goes beyond just Type 2.14
We are also investigating the potential of an oral inhibitor of Bruton's tyrosine kinase (BTK) in asthma.¹³ We are analyzing its ability to potentially lead to future reduction in symptoms and loss of asthma control events, which may result in reduction in exacerbations for patients with asthma.
Furthermore, we are investigating an asset that combines targeting of interleukin-13 (IL-13) and thymic stromal lymphopoietin (TSLP), both potentially key drivers of the inflammation in respiratory diseases like asthma, COPD and CRSwNP.¹³ A goal of our research is to determine if the combination of these targets could create better outcomes for patients than with single targets.
As part of our ongoing partnership with Regeneron, we are also exploring the potential of targeting interleukin-33 (IL-33) across COPD and other respiratory diseases.¹³ IL-33 is thought to be involved in different types of inflammation.15
Igniting the Next Wave of Innovations
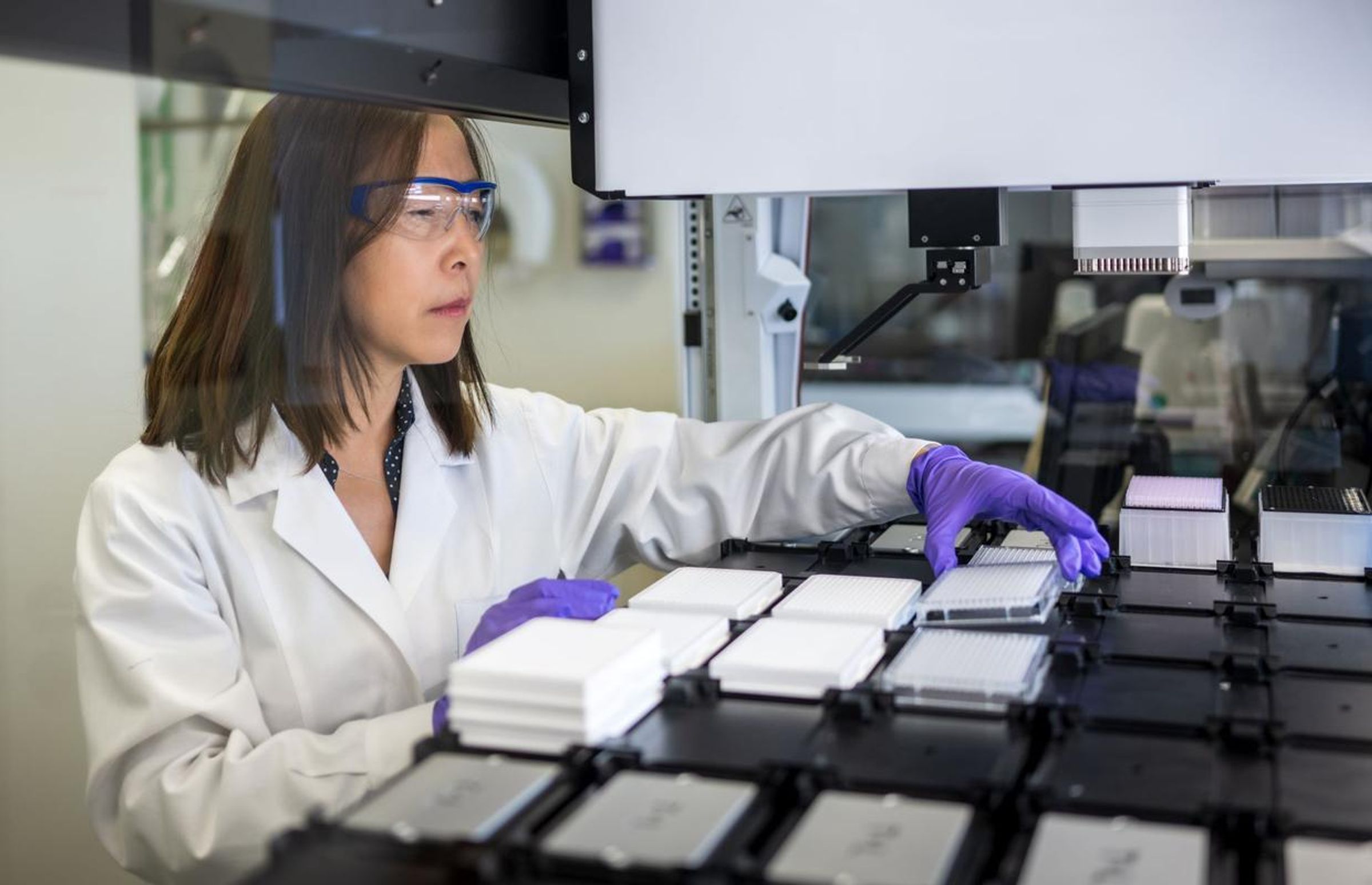
Sanofi leverages some of the best R&D technology in the form of artificial intelligence and data analysis platforms, patient-centric clinical trials and — most importantly — passionate scientists who drive our innovative spirit. Immunoscience is the bedrock of Sanofi’s research and development and enables us to apply deep biological pathway knowledge and expertise across different, often seemingly unrelated, therapeutic areas.
As we continue to chase the miracles of science and unlock the potential of the immune system, we remain driven not by what, but by who is at the center of everything we do: the patient.
“As we look ahead to the future of respiratory disease treatment, I’m inspired by new potential advancements in the space,” said Ashrafian. “They support our goal of lessening the burden of disease on patients, so they don’t have to think about their disease anymore.”
Explore More
Taking Down Type 2 Inflammatory Disease

The Next Breath: Advancing Knowledge to Transform Asthma Care
The AI Revolution in Drug Discovery: Transforming the Way We Develop New Therapies
References
- Chronic respiratory diseases - Overview. World Health Organization (WHO). 2025. Accessed October 14, 2025. https://www.who.int/health-topics/chronic-respiratory-diseases#tab=tab_1
- Chronic respiratory diseases - Symptoms. World Health Organization (WHO). 2025. Accessed October 14, 2025. https://www.who.int/health-topics/chronic-respiratory-diseases#tab=tab_2
- Asthma. World Health Organization (WHO). May 6, 2024. Accessed October 14, 2025. https://www.who.int/news-room/fact-sheets/detail/asthma
- What Is Chronic Obstructive Pulmonary Disease (COPD)? Cleveland Clinic. August 19, 2024. Accessed October 14, 2025. https://my.clevelandclinic.org/health/diseases/8709-chronic-obstructive-pulmonary-disease-copd
- Asthma Symptoms. Asthma & Allergy Foundation of America. January 2022. Accessed October 14, 2025. https://aafa.org/asthma/asthma-symptoms/
- Association AL. COPD and Emotional Health. American Lung Association. June 26, 2025. Accessed October 14, 2025. https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd/living-with-copd/coping-with-emotions
- Abu Al Karsaneh O, Al Anber A, Al Shboul S, et al. Impact of Anxiety and Depression on the Level of Asthma Control Among Jordanian Adults with Asthma. J Asthma Allergy. 2024;17:463-476. doi:10.2147/JAA.S457875
- Soler-Cataluña JJ, Huerta A, Almagro P, González-Segura D, Cosío BG. Lack of Clinical Control in COPD Patients Depending on the Target and the Therapeutic Option. Int J Chron Obstruct Pulmon Dis. 2023;18:1367-1376. doi:10.2147/COPD.S414910
- American College of Allergy, Asthma & Immunology (ACAAI). Asthma Facts. ACAAI Public Website. January 28, 2023. Accessed October 14, 2025. https://acaai.org/asthma/asthma-101/facts-stats/
- Association AL. COPD Trends Brief - Burden. American Lung Association. 2025. Accessed October 14, 2025. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief/copd-burden
- Guilleminault L, Mounié M, Sommet A, et al. The economic burden of asthma prior to death: a nationwide descriptive study. Front Public Health. 2024;12:1191788. doi:10.3389/fpubh.2024.1191788
- Sato A, Nagai H, Suzuki A, et al. Generation and characterization of OX40-ligand fusion protein that agonizes OX40 on T-Lymphocytes. Front Immunol. 2025;15. doi:10.3389/fimmu.2024.1473815
- Our Product Pipeline | Sanofi. Sanofi. July 31, 2025. Accessed October 14, 2025. https://www.sanofi.com/en/our-science/our-pipeline
- Leeuw T, Šimaitė D, Heyninck K, et al. Combined TNF-α and OX40L targeting as a new treatment option for hidradenitis suppurativa. J Allergy Clin Immunol Glob. 2025;4(3):100483. doi:10.1016/j.jacig.2025.100483
- Van der Ploeg EK, Krabbendam L, Vroman H, et al. Type-2 CD8+ T-cell formation relies on interleukin-33 and is linked to asthma exacerbations. Nat Commun. 2023;14:5137. doi:10.1038/s41467-023-40820-x