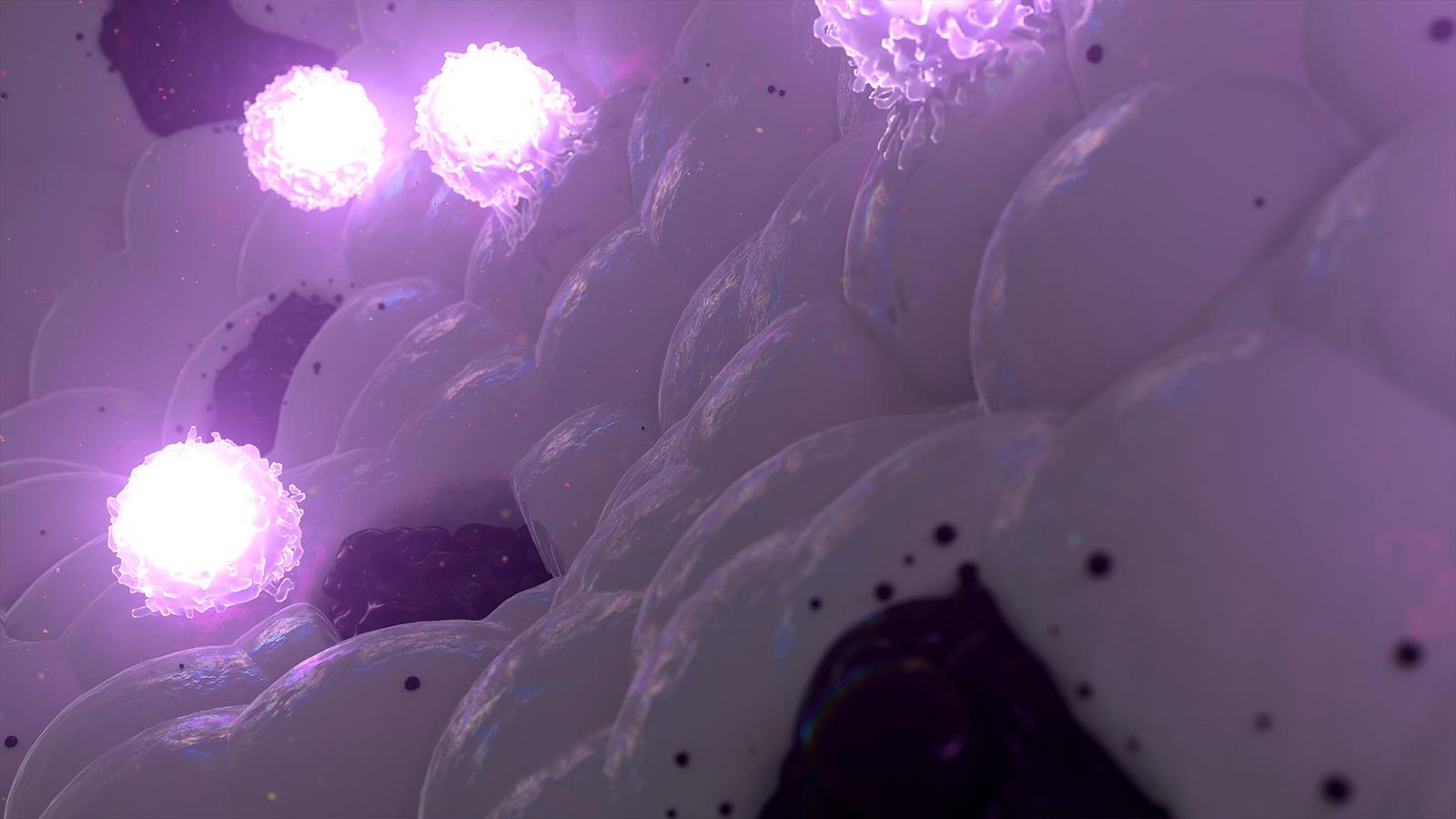
We are pioneering a new era in immunology to ignite discovery and advance innovative therapies and vaccines for patients across the spectrum of human disease.
An Ambition to Be the World Leader in Immunology
Our deep expertise in the immune system and legacy of life-changing science began more than 50 years ago when we delivered the world’s first polio vaccine. Since that time, our science has continued to set new standards of care and helped bring novel, first- and best-in-class medicines to people all over the world. But we believe we can go further. Redefining immunology as we know it, our immunoscience approach is the bedrock of Sanofi’s research and development (R&D) powerhouse.

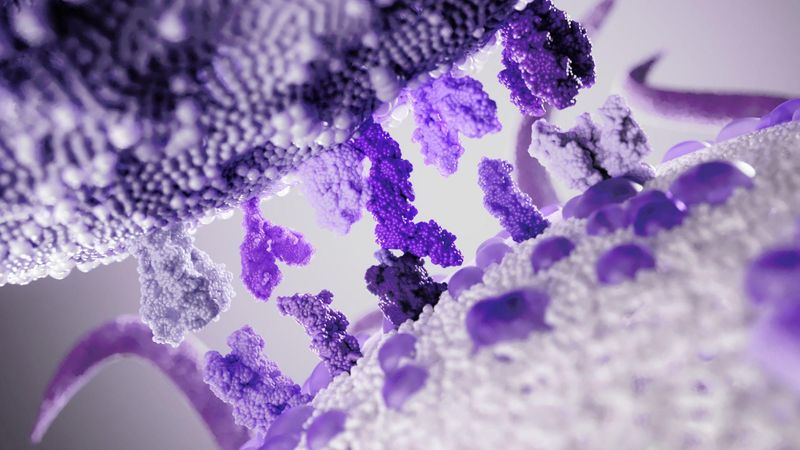
Immunoscience: a New Approach in R&D
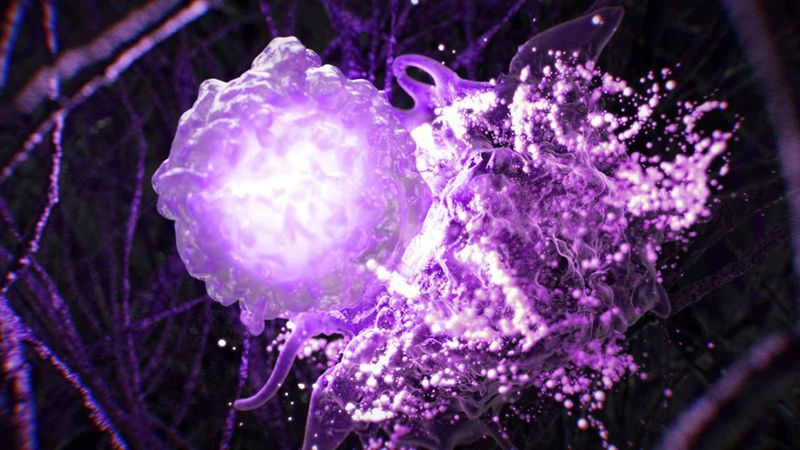
Immunoscience enables us to apply our deep knowledge and expertise beyond the boundaries of conventional immunology. It allows us to evaluate pathways of immunity and how they function independent of specific disease or pathology. This approach lays the groundwork for potential first-and best-in-class medicines that can treat a multitude of conditions across therapeutic areas so diverse, they would not have been considered to be related even a decade ago.
Powering immunoscience with artificial intelligence (AI), we are forging collaborations with the best external minds and expertise to augment our capabilities and help us drive innovation even faster. Integrating experiences and insights from patients at every step, we are accelerating the discovery and development of breakthrough medicines that will potentially help prevent and treat many more diseases, and transform more lives at a pace like never before.
Explore Our R&D Focus Areas
See how immunoscience is redefining the discovery, research and development of innovative therapies and vaccines.
Immunology
Vaccines

Neurology
Oncology

Rare Diseases
Fuelled by Technology
Our R&D is powered by innovative technologies, including a diverse range of therapeutic platforms and sophisticated computational technologies. One of these tools is AI, which allows us to tackle complex drug design and delivery challenges to bring transformative therapies to patients faster than ever before. With AI-powered immunoscience, we can increase the probability of success and expose fewer patients to unnecessary interventions.
Science and Innovation Stories
Discover breakthrough moments on our journey to becoming the world leader in immunology.
How Immunoscience is Driving the Pipeline of the Future

Digital “Twinning”: Clinical Trials Powered by AI
Every Breath Matters: Addressing Unmet Needs in Respiratory Care

Neuroimmunology Unlocks the Mysteries of the Brain
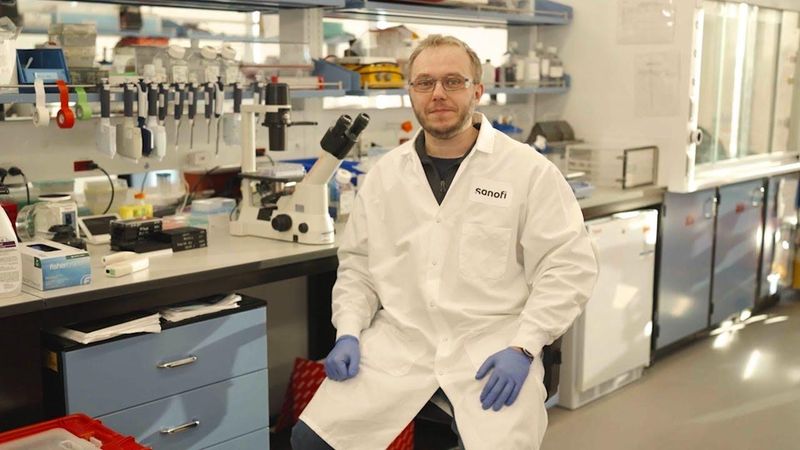
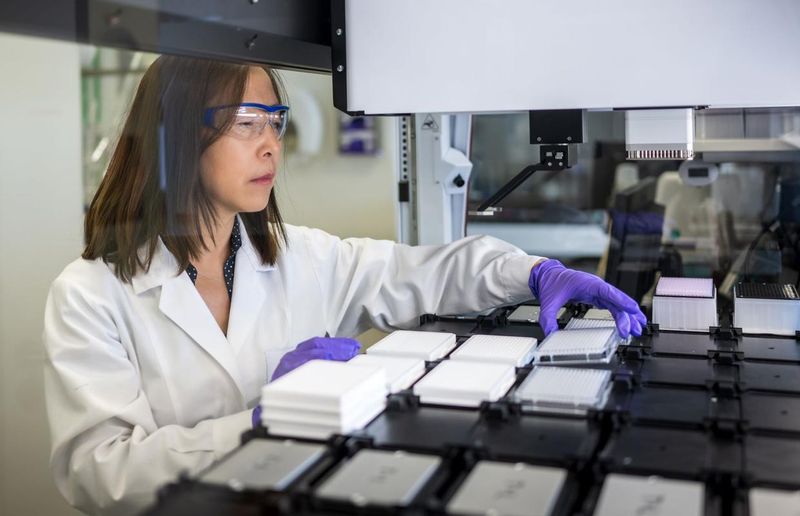
Meet Our Extraordinary Scientists
Little moments in the lab lead to big science. Listen to stories from our scientists and watch them take on the #NoJargon challenge.